Knowledge Center

Do These 3 USP 2024 Compliance Gaps Sound Familiar?
USP’s updated General Chapter <797> is now official, setting new standards for hospital pharmacies. But are you ready?
Checklists Are a Must
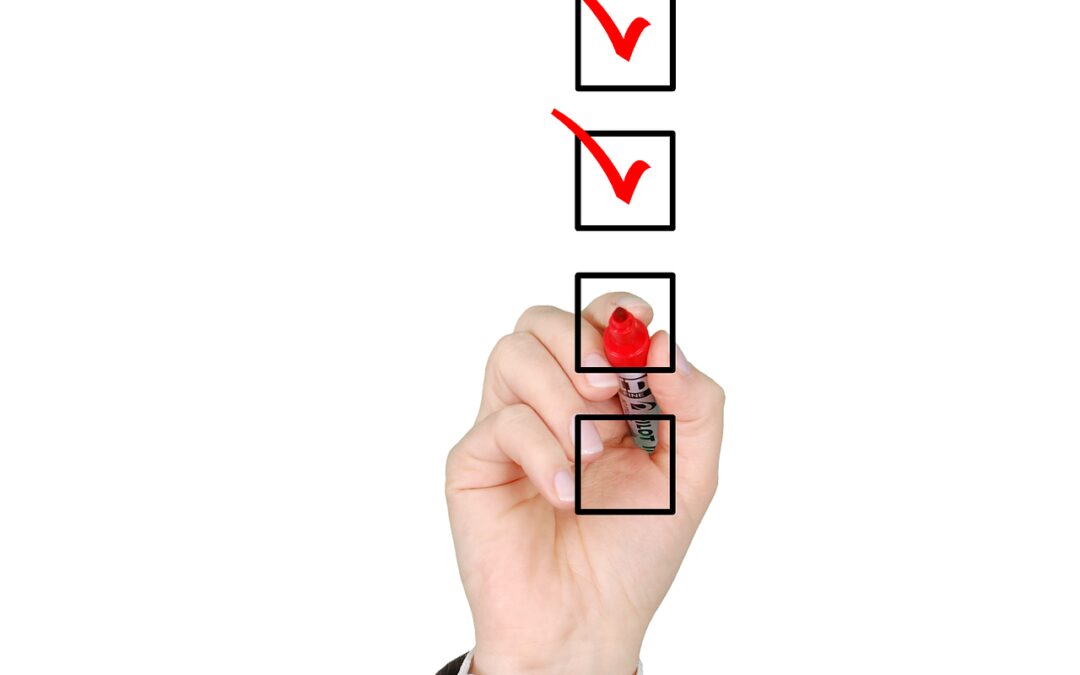
In his book The Checklist Manifesto, Atul Gawande does a great job explaining why checklists are required for success.

How “Scope Creep” Can Save Health Care
🚨Important Read Alert: Addressing Misconceptions About Pharmacists' Role🚨An article from the American Medical Association, authored by Timothy M. Smith sparked debate on social media, questioning the role of pharmacists in...

Start with Optimizing Team Resources
Pharmacy technicians have a wide range of critical responsibilities that directly impact patient care and the pharmacy’s compliance with regulations and best practices. It’s no secret that many pharmacies continue to have a difficult time recruiting and retaining...

RFID Technology Transforms Pharmacy Management
Embracing RFID technology transforms pharmacy management with applications in inventory control, medication authentication, patient adherence, and workflow efficiency. RFID tags on medication containers enable real-time tracking, automating reorder processes to...

FDA’s Traceability Final Rule
The global supply chain faces challenges, leading to product shortages and delays. The food industry, impacted by these issues, is undergoing a digital transformation to enhance supply chain visibility. The U.S. FDA's Traceability Final Rule focuses on improving...

Compounders Pathways for BUDS in revised USP <797> Chapter.
The revised USP General Chapter <797> offers compounders pathways for extended beyond-use dates (BUDs) in sterile preparations, with increasing BUDs tied to stricter requirements. Compliance is emphasized as a continuous journey, according to Kevin Hansen, PharmD....

Ensuring Compliance With USP 795 Nonsterile Compounding
US pharmacies are at risk of compromising patient safety by not giving enough attention to nonsterile compounding standards (USP General Chapter <795>). With a focus on sterile compounding and hazardous drug handling, many pharmacies are unprepared for the upcoming...

Office of Inspector General has new comprehensive compliance program guidance (GCPG)!
The U.S. Department of Health and Human Services' Office of Inspector General has issued new comprehensive compliance program guidance (GCPG) for the healthcare compliance community. This guidance applies across all healthcare stakeholders, including providers,...

How Does Your Hospital Rank?
If you are a hospital, it’s time to talk about your grades. Every year hospitals are evaluated and rated by outside organizations, with two of the most important being the hospital Star Ratings by the Centers for Medicare & Medicaid Services (CMS) and Best...

Do These 3 USP 2024 Compliance Gaps Sound Familiar?
🔍 Dive into the New Era of Sterile Compounding! 🧪💉 USP’s updated General Chapter <797> is now official, setting new standards for hospital pharmacies. But are you ready for the Joint Commission and other state/ federal agency inspections based on these requirements? Here are some common compliance gaps:
1️ Environmental Monitoring and Cleaning: Monthly surface sampling is now a must, but many struggle with inadequate sampling or improper cleaning solutions.
2️ Understanding Required Competencies: Garbing and aseptic manipulation competency evaluations are crucial every six months, but confusion still persists in certain areas, such as the order of specific aseptic manipulation steps.
3️ Cut-and-Paste SOPs: Generic SOPs won’t cut it. Tailor your procedures with clear, specific details to ensure compliance.
Don’t let compliance gaps jeopardize patient safety! Stay informed, train your team, and take charge of your processes. The Joint Commission and state/federal agencies are watching closely. 💼💡Full article #SterileCompounding #PharmacyPractice #PatientSafety #Katanarx #terlumina #USPstandards #usp797 #saas #pharmacycompliance

Checklists Are a Must
✔ If you work with complexity (e.g., healthcare) and have not read this book, you should.
✔ If you have not implemented a checklist strategy, you must.
“under conditions of complexity, not only are checklists a help, they are required for success. There must always be room for judgment, but judgment aided—and even enhanced—by procedure.” – Atul Gawande
Terlumina provides supercharged task-based checklists that ensure transparency, accountability, diligence, and operational optimization.
Don’t wait, contact us now.

How “Scope Creep” Can Save Health Care
🚨Important Read Alert: Addressing Misconceptions About Pharmacists’ Role🚨
An article from the American Medical Association, authored by Timothy M. Smith sparked debate on social media, questioning the role of pharmacists in healthcare. While acknowledging pharmacists’ importance, it emphasized physicians as leaders, dismissing collaborative efforts.
However, Smith’s stance overlooks pharmacists’ extensive training, including board certification and residency programs, spanning various specialties. Pharmacists offer crucial patient care beyond medication expertise, impacting outcomes positively.
In her recent article, “How “Scope Creep” Can Save Health Care”, Lauren Massaro focuses on Smith’s oversight regarding pharmacists’ role by diving into how legislation expanding pharmacists’ scope has proven beneficial, especially evident during the COVID-19 pandemic. She deals herself a great hand against the opinion of Smith’s article and emphasizes on how collaborative models enhance patient care and alleviate healthcare burdens!
Let’s focus on teamwork and patient-centered care, leveraging the strengths of both professions for better health outcomes.

https://www.drugtopics.com/view/how-scope-creep-can-save-health-care

Start with Optimizing Team Resources
Pharmacy technicians have a wide range of critical responsibilities that directly impact patient care and the pharmacy’s compliance with regulations and best practices. It’s no secret that many pharmacies continue to have a difficult time recruiting and retaining trained pharmacy technicians, and many hospitals and health systems are experiencing severe shortages resulting in increased risk. Just last month, an article published in the ASHP News Center reported how Children’s Hospital Colorado (CHCO), a health system serving seven states, has struggled due to the inability to increase pharmacy technician salaries to make the positions more enticing. A 2022 ASHP survey indicated that technicians expressed frustration with workload, work schedules, and pay. Most agree that this problem is not going away anytime soon, and many approaches have been taken to try and alleviate it, including apprenticeship programs, career enhancement initiatives, and of course increasing pay and benefits when feasible. One fundamental strategy, however, that can form the foundation for all other approaches is having a framework in place that empowers and optimizes your current team. KatanaRX is the task-based framework for accomplishing this. It allows you to optimize team resources by actually streamlining operations instead of disrupting them.


RFID Technology Transforms Pharmacy Management
Embracing RFID technology transforms pharmacy management with applications in inventory control, medication authentication, patient adherence, and workflow efficiency. RFID tags on medication containers enable real-time tracking, automating reorder processes to prevent shortages. Ensuring medication authenticity, RFID enhances patient safety by minimizing counterfeit drugs in the supply chain. RFID-enabled packaging promotes patient adherence through automated reminders, improving health outcomes. The technology also streamlines pharmacy workflows, automating tasks, reducing errors, and updating electronic health records. RFID brings benefits like improved patient safety, enhanced efficiency, cost savings, compliance, and real-time visibility, making it indispensable in modern pharmacy operations. Ongoing advancements position RFID as a central tool shaping the future of pharmacy, ultimately elevating patient care and outcomes. More Info here!
#RFIDTechnology #PharmacyManagement #PatientSafety #HealthTech #Innovation

FDA’s Traceability Final Rule
The global supply chain faces challenges, leading to product shortages and delays. The food industry, impacted by these issues, is undergoing a digital transformation to enhance supply chain visibility. The U.S. FDA’s Traceability Final Rule focuses on improving product traceability, requiring additional record keeping for high-risk foods. GS1 Standards, such as GTINs and GLNs, play a crucial role in implementing traceability programs. Quality data management is vital, ensuring accurate, standardized information for efficient communication. The adoption of advanced data carriers, like 2D barcodes and RFID, facilitates transparency and traceability. Industry initiatives, such as Sunrise 2027, aim to implement advanced barcode scanning within four years. With the Traceability Final Rule deadline approaching in 2026, now is the time to prioritize traceability and supply chain visibility. View full article information here!
#SupplyChain #Traceability #FoodSafety #GS1Standards

Compounders Pathways for BUDS in revised USP <797> Chapter.
The revised USP General Chapter <797> offers compounders pathways for extended beyond-use dates (BUDs) in sterile preparations, with increasing BUDs tied to stricter requirements. Compliance is emphasized as a continuous journey, according to Kevin Hansen, PharmD. The revised chapter categorizes sterile compounding into three groups, simplifying determination based on preparation environment. Category 1 allows flexibility, with BUDs of up to 24 hours if refrigerated. Category 2 involves greater processing rigor for longer-lasting medications, while Category 3 permits a maximum BUD of 180 days under frozen conditions, with strict controls corresponding to the level of risk. Considerations for each category provide guidance for compounding pharmacists. Check out full article information here.
#USP797 #SterileCompounding #PharmacyPractices

Ensuring Compliance With USP 795 Nonsterile Compounding
US pharmacies are at risk of compromising patient safety by not giving enough attention to nonsterile compounding standards (USP General Chapter <795>). With a focus on sterile compounding and hazardous drug handling, many pharmacies are unprepared for the upcoming nonsterile compounding guidelines effective from November 1, 2023. Pharmacists should assess if nonsterile compounding takes place in their facility, ensuring compliance with scope, purchase history, and dispense history. Properly equipping designated areas and equipment is crucial. Staff must be well-trained and competent in nonsterile compounding, with regular training, cleaning, and documentation to meet the new standards. Terlumina operationalizes the assessments needed and helps pharmacies achieve compliance for success in meeting these newest USP standards. Stay updated here!

Office of Inspector General has new comprehensive compliance program guidance (GCPG)!
The U.S. Department of Health and Human Services’ Office of Inspector General has issued new comprehensive compliance program guidance (GCPG) for the healthcare compliance community. This guidance applies across all healthcare stakeholders, including providers, managed care plans, pharmaceutical manufacturers, and service providers. The GCPG is a voluntary resource emphasizing best practices rather than mandatory requirements. It encourages the inclusion of quality and patient safety in compliance programs, provides insights into fraud, waste, and abuse laws, highlights common risk areas, clarifies the role of compliance officers, promotes incentives for compliance, and offers adaptations for small entities. The GCPG also addresses nontraditional service providers, new players in healthcare, and evolving payment structures. Overall, it aims to improve and update existing compliance guidance for the healthcare industry. Stay up to date on the new GCPG here.

How Does Your Hospital Rank?
If you are a hospital, it’s time to talk about your grades. Every year hospitals are evaluated and rated by outside organizations, with two of the most important being the hospital Star Ratings by the Centers for Medicare & Medicaid Services (CMS) and Best Hospitals ranking by U.S. News & World Reports.
CMS’s overall star ratings are based on forty-six quality measures in five categories: mortality, safety, readmission, patient experience, and timely/effective care. Each overall rating shows how well the hospital performed on these quality measures compared to other hospitals in the U.S. The more stars, the better a hospital performed.
U.S. News & World Report’s rankings, in turn, are broken into two subcomponents: specialty rankings and procedure and condition ratings. Specialty rankings are intended for those with life-threatening or rare conditions needing top-level care for complex cases. Procedure and condition ratings focus on commonly needed procedures or conditions (e.g., hip replacement, heart failure). For both subcomponents, the ratings are based on quality of care with a focus on the relationship between structure (hospital resources connected with patient care), process (the way in which diagnoses, treatments, and practices are built into routine), and outcomes (the results of the care).
Not surprisingly, hospitals often turn to external expert consultants to help them achieve a better ranking/rating. Typically, these consultants provide a gap analysis to identify opportunities for improvement along with specific recommendations in the form of corrective actions and best practices to be taken. These recommendations may range from policy/procedure changes to operational processes and steps based on these policies/procedures to be taken.
While expert recommendations can be a great step, many hospitals still do not achieve the ranking/rating they hoped for, or if they do are unable to sustain it over time. Why? The answer is simple really. No matter how detailed corrective action and best practice recommendations are, each step must be operationally implemented and consistently performed. In actual practice, this is much more difficult than it sounds. The key is establishing an operational infrastructure that ensures transparency, accountability, and unrelenting diligence from the top down –without increasing daily workload or making things more complicated. Terlumina provides a single, powerful enterprise-wide solution that simplifies the process. Proactively monitor compliance metrics and key performance indicators (KPIs) based on tasks and assessments. Target identified risks, implement corrective actions, and objectively measure improvement.

Do These 3 USP 2024 Compliance Gaps Sound Familiar?
🔍 Dive into the New Era of Sterile Compounding! 🧪💉 USP’s updated General Chapter <797> is now official, setting new standards for hospital pharmacies. But are you ready for the Joint Commission and other state/ federal agency inspections based on these requirements? Here are some common compliance gaps:
1️ Environmental Monitoring and Cleaning: Monthly surface sampling is now a must, but many struggle with inadequate sampling or improper cleaning solutions.
2️ Understanding Required Competencies: Garbing and aseptic manipulation competency evaluations are crucial every six months, but confusion still persists in certain areas, such as the order of specific aseptic manipulation steps.
3️ Cut-and-Paste SOPs: Generic SOPs won’t cut it. Tailor your procedures with clear, specific details to ensure compliance.
Don’t let compliance gaps jeopardize patient safety! Stay informed, train your team, and take charge of your processes. The Joint Commission and state/federal agencies are watching closely. 💼💡Full article #SterileCompounding #PharmacyPractice #PatientSafety #Katanarx #terlumina #USPstandards #usp797 #saas #pharmacycompliance

Checklists Are a Must
✔ If you work with complexity (e.g., healthcare) and have not read this book, you should.
✔ If you have not implemented a checklist strategy, you must.
“under conditions of complexity, not only are checklists a help, they are required for success. There must always be room for judgment, but judgment aided—and even enhanced—by procedure.” – Atul Gawande
Terlumina provides supercharged task-based checklists that ensure transparency, accountability, diligence, and operational optimization.
Don’t wait, contact us now.

How “Scope Creep” Can Save Health Care
🚨Important Read Alert: Addressing Misconceptions About Pharmacists’ Role🚨
An article from the American Medical Association, authored by Timothy M. Smith sparked debate on social media, questioning the role of pharmacists in healthcare. While acknowledging pharmacists’ importance, it emphasized physicians as leaders, dismissing collaborative efforts.
However, Smith’s stance overlooks pharmacists’ extensive training, including board certification and residency programs, spanning various specialties. Pharmacists offer crucial patient care beyond medication expertise, impacting outcomes positively.
In her recent article, “How “Scope Creep” Can Save Health Care”, Lauren Massaro focuses on Smith’s oversight regarding pharmacists’ role by diving into how legislation expanding pharmacists’ scope has proven beneficial, especially evident during the COVID-19 pandemic. She deals herself a great hand against the opinion of Smith’s article and emphasizes on how collaborative models enhance patient care and alleviate healthcare burdens!
Let’s focus on teamwork and patient-centered care, leveraging the strengths of both professions for better health outcomes.

https://www.drugtopics.com/view/how-scope-creep-can-save-health-care

Start with Optimizing Team Resources
Pharmacy technicians have a wide range of critical responsibilities that directly impact patient care and the pharmacy’s compliance with regulations and best practices. It’s no secret that many pharmacies continue to have a difficult time recruiting and retaining trained pharmacy technicians, and many hospitals and health systems are experiencing severe shortages resulting in increased risk. Just last month, an article published in the ASHP News Center reported how Children’s Hospital Colorado (CHCO), a health system serving seven states, has struggled due to the inability to increase pharmacy technician salaries to make the positions more enticing. A 2022 ASHP survey indicated that technicians expressed frustration with workload, work schedules, and pay. Most agree that this problem is not going away anytime soon, and many approaches have been taken to try and alleviate it, including apprenticeship programs, career enhancement initiatives, and of course increasing pay and benefits when feasible. One fundamental strategy, however, that can form the foundation for all other approaches is having a framework in place that empowers and optimizes your current team. KatanaRX is the task-based framework for accomplishing this. It allows you to optimize team resources by actually streamlining operations instead of disrupting them.


RFID Technology Transforms Pharmacy Management
Embracing RFID technology transforms pharmacy management with applications in inventory control, medication authentication, patient adherence, and workflow efficiency. RFID tags on medication containers enable real-time tracking, automating reorder processes to prevent shortages. Ensuring medication authenticity, RFID enhances patient safety by minimizing counterfeit drugs in the supply chain. RFID-enabled packaging promotes patient adherence through automated reminders, improving health outcomes. The technology also streamlines pharmacy workflows, automating tasks, reducing errors, and updating electronic health records. RFID brings benefits like improved patient safety, enhanced efficiency, cost savings, compliance, and real-time visibility, making it indispensable in modern pharmacy operations. Ongoing advancements position RFID as a central tool shaping the future of pharmacy, ultimately elevating patient care and outcomes. More Info here!
#RFIDTechnology #PharmacyManagement #PatientSafety #HealthTech #Innovation

FDA’s Traceability Final Rule
The global supply chain faces challenges, leading to product shortages and delays. The food industry, impacted by these issues, is undergoing a digital transformation to enhance supply chain visibility. The U.S. FDA’s Traceability Final Rule focuses on improving product traceability, requiring additional record keeping for high-risk foods. GS1 Standards, such as GTINs and GLNs, play a crucial role in implementing traceability programs. Quality data management is vital, ensuring accurate, standardized information for efficient communication. The adoption of advanced data carriers, like 2D barcodes and RFID, facilitates transparency and traceability. Industry initiatives, such as Sunrise 2027, aim to implement advanced barcode scanning within four years. With the Traceability Final Rule deadline approaching in 2026, now is the time to prioritize traceability and supply chain visibility. View full article information here!
#SupplyChain #Traceability #FoodSafety #GS1Standards

Compounders Pathways for BUDS in revised USP <797> Chapter.
The revised USP General Chapter <797> offers compounders pathways for extended beyond-use dates (BUDs) in sterile preparations, with increasing BUDs tied to stricter requirements. Compliance is emphasized as a continuous journey, according to Kevin Hansen, PharmD. The revised chapter categorizes sterile compounding into three groups, simplifying determination based on preparation environment. Category 1 allows flexibility, with BUDs of up to 24 hours if refrigerated. Category 2 involves greater processing rigor for longer-lasting medications, while Category 3 permits a maximum BUD of 180 days under frozen conditions, with strict controls corresponding to the level of risk. Considerations for each category provide guidance for compounding pharmacists. Check out full article information here.
#USP797 #SterileCompounding #PharmacyPractices

Ensuring Compliance With USP 795 Nonsterile Compounding
US pharmacies are at risk of compromising patient safety by not giving enough attention to nonsterile compounding standards (USP General Chapter <795>). With a focus on sterile compounding and hazardous drug handling, many pharmacies are unprepared for the upcoming nonsterile compounding guidelines effective from November 1, 2023. Pharmacists should assess if nonsterile compounding takes place in their facility, ensuring compliance with scope, purchase history, and dispense history. Properly equipping designated areas and equipment is crucial. Staff must be well-trained and competent in nonsterile compounding, with regular training, cleaning, and documentation to meet the new standards. Terlumina operationalizes the assessments needed and helps pharmacies achieve compliance for success in meeting these newest USP standards. Stay updated here!

Office of Inspector General has new comprehensive compliance program guidance (GCPG)!
The U.S. Department of Health and Human Services’ Office of Inspector General has issued new comprehensive compliance program guidance (GCPG) for the healthcare compliance community. This guidance applies across all healthcare stakeholders, including providers, managed care plans, pharmaceutical manufacturers, and service providers. The GCPG is a voluntary resource emphasizing best practices rather than mandatory requirements. It encourages the inclusion of quality and patient safety in compliance programs, provides insights into fraud, waste, and abuse laws, highlights common risk areas, clarifies the role of compliance officers, promotes incentives for compliance, and offers adaptations for small entities. The GCPG also addresses nontraditional service providers, new players in healthcare, and evolving payment structures. Overall, it aims to improve and update existing compliance guidance for the healthcare industry. Stay up to date on the new GCPG here.

How Does Your Hospital Rank?
If you are a hospital, it’s time to talk about your grades. Every year hospitals are evaluated and rated by outside organizations, with two of the most important being the hospital Star Ratings by the Centers for Medicare & Medicaid Services (CMS) and Best Hospitals ranking by U.S. News & World Reports.
CMS’s overall star ratings are based on forty-six quality measures in five categories: mortality, safety, readmission, patient experience, and timely/effective care. Each overall rating shows how well the hospital performed on these quality measures compared to other hospitals in the U.S. The more stars, the better a hospital performed.
U.S. News & World Report’s rankings, in turn, are broken into two subcomponents: specialty rankings and procedure and condition ratings. Specialty rankings are intended for those with life-threatening or rare conditions needing top-level care for complex cases. Procedure and condition ratings focus on commonly needed procedures or conditions (e.g., hip replacement, heart failure). For both subcomponents, the ratings are based on quality of care with a focus on the relationship between structure (hospital resources connected with patient care), process (the way in which diagnoses, treatments, and practices are built into routine), and outcomes (the results of the care).
Not surprisingly, hospitals often turn to external expert consultants to help them achieve a better ranking/rating. Typically, these consultants provide a gap analysis to identify opportunities for improvement along with specific recommendations in the form of corrective actions and best practices to be taken. These recommendations may range from policy/procedure changes to operational processes and steps based on these policies/procedures to be taken.
While expert recommendations can be a great step, many hospitals still do not achieve the ranking/rating they hoped for, or if they do are unable to sustain it over time. Why? The answer is simple really. No matter how detailed corrective action and best practice recommendations are, each step must be operationally implemented and consistently performed. In actual practice, this is much more difficult than it sounds. The key is establishing an operational infrastructure that ensures transparency, accountability, and unrelenting diligence from the top down –without increasing daily workload or making things more complicated. Terlumina provides a single, powerful enterprise-wide solution that simplifies the process. Proactively monitor compliance metrics and key performance indicators (KPIs) based on tasks and assessments. Target identified risks, implement corrective actions, and objectively measure improvement.
The Latest
-
Do These 3 USP 2024 Compliance Gaps Sound Familiar?
-
Checklists Are a Must
-
How “Scope Creep” Can Save Health Care
-
Start with Optimizing Team Resources
-
RFID Technology Transforms Pharmacy Management
-
FDA’s Traceability Final Rule
-
Compounders Pathways for BUDS in revised USP <797> Chapter.
-
Ensuring Compliance With USP 795 Nonsterile Compounding
-
Office of Inspector General has new comprehensive compliance program guidance (GCPG)!
-
How Does Your Hospital Rank?
